In recent days and weeks, there have been statements made about moving from a COVID-19 pandemic state to an endemic phase by the end of October 2021. The argument for this is higher adult vaccination rates that will be achieved nationwide by that time period.
So we need to ask this question: Is Malaysia ready to move to an endemic phase by the end of October 2021?
I would like to describe some ‘movements’ we need to make as a nation for us to be ready to enter an endemic phase, as well as offer you a ‘report card’ of our preparedness measures.
Move from Looking at Adult Vaccination Rates to Total Population Vaccination Rates
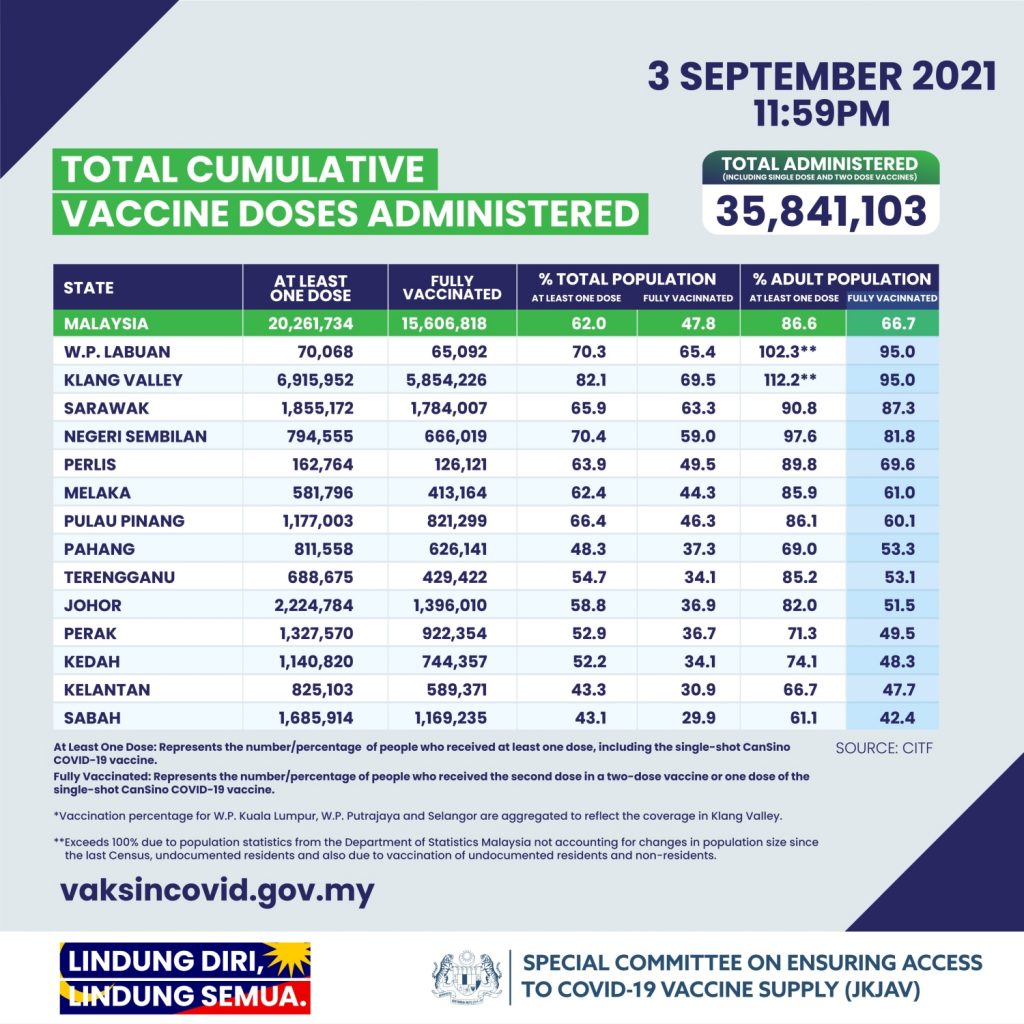
The data from many countries is very clear that the virus continues to spread as long as you have segments of your population that are unvaccinated; especially children. Hence it is important that we stop talking or showing data on adult vaccination rates and concentrate only on total population vaccination rates. For example, even in regions with high vaccination coverage, the total vaccination rates are below 70% currently (CITF data 3rd September: Klang Valley 69.5%, Sarawak 63.3%). We need 90% of the community vaccinated to move to an endemic phase (see next section).
Move away from Herd Immunity Concepts to Mitigating Outbreaks
The Delta variant has changed the entire landscape of the COVID-19 pandemic. It is clear that we will have breakthrough infections in those fully vaccinated; fortunately, the majority will be mild. Current CDC and PHE data suggest that vaccination (mRNA and adenovirus vaccines) reduce the risk of breakthrough infections with Delta 3X and reduce the risk of severe disease or death by 10X (data for Sinovac protection against Delta is still very limited but may be lower). Hence we should expect that 1 in 3 persons vaccinated with a mRNA or adenovirus vaccine can get a breakthrough infection and have the potential to infect those who are not vaccinated.
This is why herd immunity is no longer possible and why we need high levels of total population vaccination. Good models have shown that to open up any society (reach an endemic state) we require close to 90% vaccination rates of the population. Australian National University modelling shows that even if 70% of adults are vaccinated they can expect 6.9 million cases, 154,000 hospitalisations and 29,000 deaths. Australia needs a 90% vaccination target (including children) before moving to the final stage of the national plan (opening up fully). Even with 90% of the population vaccinated they expect 5,000 fatalities and 40,000 cases of long COVID.
Hence even when we move to high total population vaccination rates, we still need to keep in place the key public health mitigation measures – routine mask use, reduced social interaction, physical distancing, significant improvements in indoor ventilation and routine testing strategies. Even in an endemic phase with high vaccination rates we need to reduce COVID-19 transmission to minimise some getting ill and reduce the risk of new variants of concern developing.
Move from Vaccinating Adults to Vaccinating Children (Before Re-opening Schools)
We must realise that if we open up too quickly we run the risk of large outbreaks, especially in children. This can be seen currently in Norway, the United States and the United Kingdom where children have returned to school. We are aware that the Delta variant is far more infectious and 2x move severe. The United States and the United Kingdom are currently reporting sizable numbers of children admitted (1% of infections) and many of the paediatric intensive care units (PICUs) are getting overrun. Locally my paediatric colleagues have been expressing concern about the increase they are seeing of ill children with COVID-19 due to the Delta wave. The number of children with severe multisystem inflammatory syndrome (MIS-C) due to COVID-19 is no longer uncommon. Our PICU development in Malaysia has been even worse than that of adult ICUs. If we open up quickly into an ‘endemic phase’ and allow schools to open as planned (October 2021), we will definitely be overrun and the childhood mortality from COVID-19 will rise (as happened in Indonesia). We must boost our children’s ICU capacity now before we are overrun.
We have to vaccinate children aged 12-17 years before they return to school. Vaccine supply is an issue as many adults outside the Klang valley have yet to get a dose. As soon as it is possible we should offer vaccines to our teenagers. Meanwhile, we should be careful and maintain vigilance for all children. The problem will be the children aged 5 to 11 years and those under 5 years of age. There is currently no data available on the safety of vaccines in these age groups and we will have to wait for clinical trial results. The Delta variant can harm children under 5 years with hospitalisations rates as high as adolescents aged 12–17 years. We need the Ministry of Health to closely monitor the trend in children and provide disaggregated data to the public. We must move away from aggregated data that lumps past outcomes with present outcomes as we need to see the Delta effect and the impact over time. So we need to see monthly data on infected children by severity, age and state.
Move from SOPs to a Sustainable Change in Lifestyle. Move from External Enforcement to Societal Checks. Move from a Dependence on Vaccines Alone to Using All Tools & Mitigation Measures
I have put these areas together as they are interrelated. For some time now the subtle message has been that “vaccines will be the silver bullet in this pandemic”. It is clear that this is not the case as new variants develop. The health services must continue to use all public health tools at our disposal and heighten all mitigation measures. Currently, the support for our public health staff is poor.
The movement we must make is away from the protean and laborious standard operating policies (SOPs) to a sustainable lifestyle change. This must be associated with a decrease in enforcement by the authorities (police) and an increase of society policing itself. No person (unless with a medical reason) should be allowed to move around without a mask and all of us should ‘call them out’ if they do so (including mask-chinians and nose-maskians). All of us should actively work to improve indoor ventilation at shops, school classrooms, offices, factories, gyms, etc. Society must actively decry (criticise and discourage) unnecessary and large social interactions.
At all times we must realise we are in this together. If we do not help the poor and migrants, we do so at our peril. How COVID-19 evolves depends on our collective behaviour and supporting each other is critical.
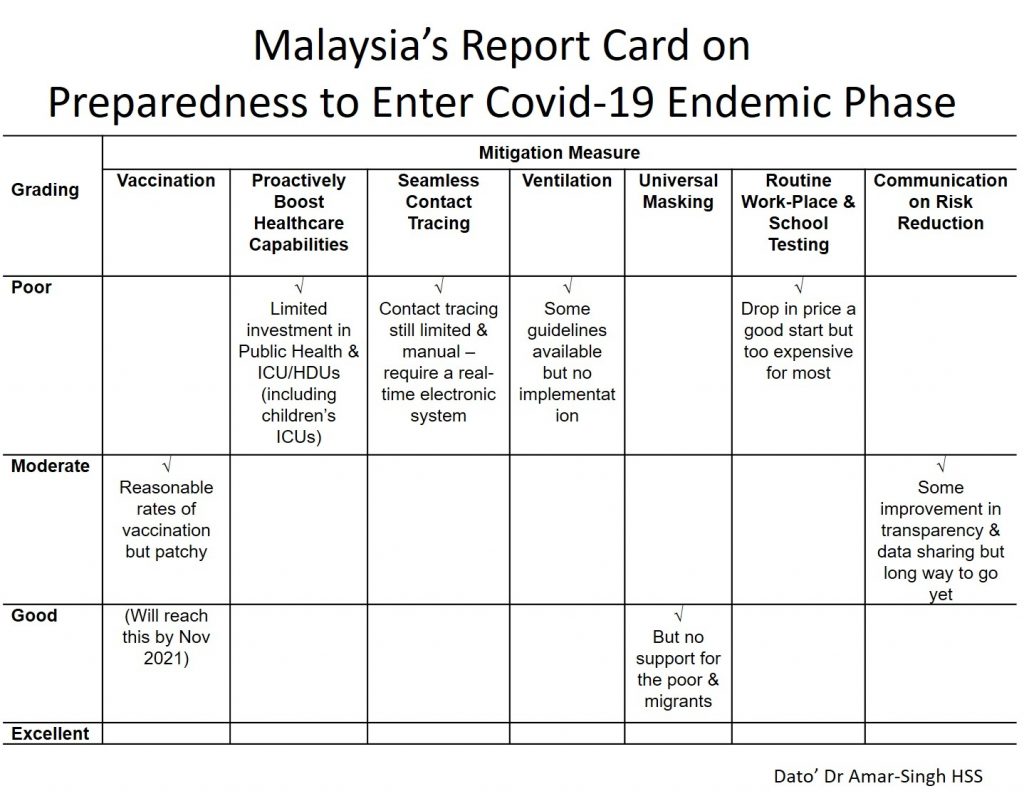
Malaysia’s Report Card on Preparedness to Enter a COVID-19 Endemic Phase
The table below shows an assessment of our nation’s preparedness to enter a COVID-19 endemic phase. It can be seen that we are not ready and have much work to do. We must ramp up our initiatives and support if we are to consider entering an endemic phase by January or February 2022 (when national vaccination rates reach 80% and teenagers have been vaccinated). Schools must put in place vital measures to protect children before they open. All this is assuming we do not see new variants appearing that are partially or fully resistant to vaccine induce immunity.
Three Possible ‘Phases’ Impending
Finally, a note about what is coming. No one can predict what will happen with COVID-19 but listening to many international experts and looking at our situation I would like to offer some ideas (see the Figure below).
We are currently in what I call the ‘Primary Protection Phase’ where we are racing against Delta and trying to complete adult vaccination. Many states outside the Klang valley are in trouble and we are starting to see rising cases of children hospitalised nationally.
We will then move to what I call a ‘Consolidation Phase’ where we try to increase societal protection and reduce the spread of COVID-19 by vaccination of teenagers. Meanwhile, we have to look hard at the data for any signs of waning immunity and if adult boosters are required.
We then enter a phase I have chosen to intentionally call the ‘Long-term Danger Phase’. Here is where we must not let down our guard and risk more outbreaks, especially if worse variants appear. We can do this by a change in lifestyle to address the long term COVID-19 journey. There may be a need to invest in new vaccines.
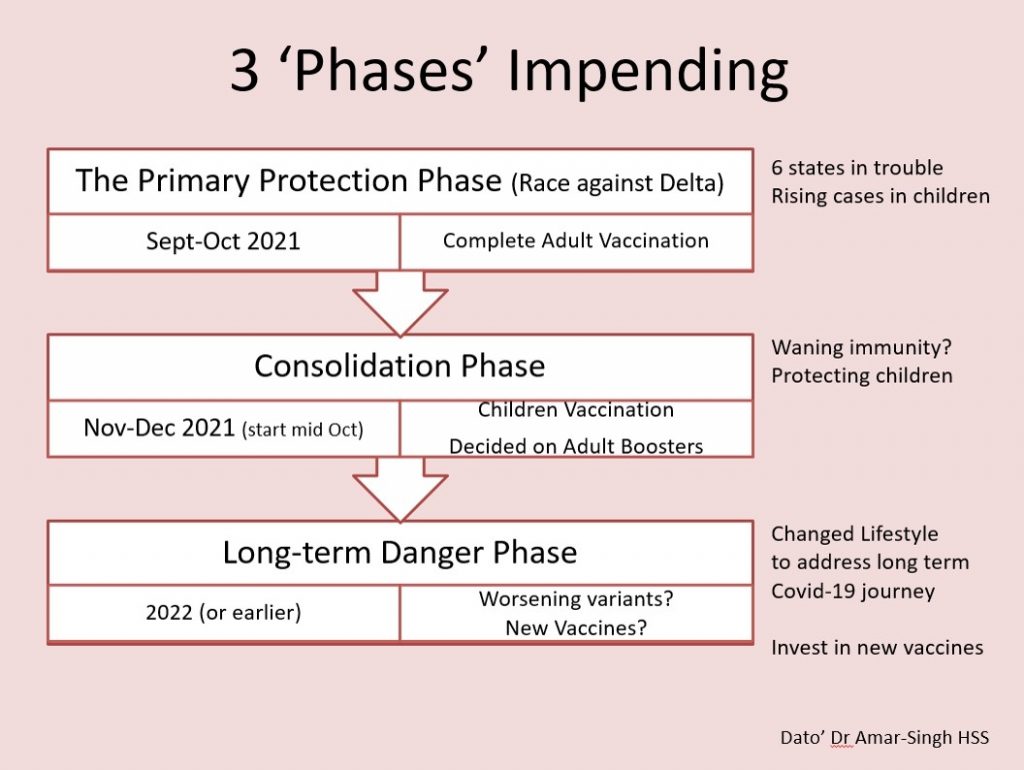
Lifting restrictions and moving to an ‘endemic’ phase does not mean we do not maintain routine mask use or return to pre-COVID social interactions. We need to maintain caution even with adequate vaccination. The COVID-19 virus will exploit all weaknesses in human behaviour and hence we need to always work together.
This opinion piece was contributed by Dato’ Dr Amar-Singh HSS, Senior Consultant Paediatrician. If you have an article or opinion that you would like to contribute for the benefit everyone, share it with us here.
0 comments :
Post a Comment